| |
| |
Apr 02, 2025
|
|
|
|
|
Undergraduate Calendar 2023-2024 [-ARCHIVED CALENDAR-]
Undergraduate Medical (MD) Program
|
|
 Return to: Programs (by Degree) and Minors Return to: Programs (by Degree) and Minors
The three-year program in Medicine uses a problem-based approach to learning that should apply throughout the physician’s career. The components have been organized in sequential blocks with early exposure to patients and case management.
|
Undergraduate MD Program Goals
The Undergraduate MD Program at McMaster University fosters a cooperative, supportive and respectful environment. The curriculum evolves continuously, responsive to the changing needs of Ontario society, nurturing the development of the following competencies at the time of graduation: - Medical Expert: Students will be able to apply scientific principles from human biology, behaviour and population health to the solution of health problems; they will have the ability to seek out new information and evaluate this information critically.
- Communicator/Collaborator: Students will demonstrate effective communication skills, sensitive to the needs of patients and cognizant of the roles of other members of the health care team in delivering patient care.
- Advocate/Resource Manager: Graduating students will be knowledgeable about the determinants of health and be proactive advocates for their individual patients and for healthy public policy within the context of the health care system.
- Scholar/Learner: Students will be self-directed lifelong learners, whose exposure at McMaster to role models in research and clinical care will encourage them to apply innovative approaches to solving health care problems.
- Self-Reflective Practitioner: Graduating students will be expected to have developed an awareness of the influence of their attitudes, values and assumptions, how these affect their practice of medicine and the impact of the practice of medicine on themselves as individuals.
The specific competencies in which students will be trained and that students must demonstrate by completion of the program can be found here: https://mdprogram.mcmaster.ca/md-
program/our-curriculum/what-is-compass. The Pre-Clerkship Curriculum
The Pre-Clerkship curriculum focuses on the mastery of fundamental concepts in medicine. It continues the McMaster tradition of Problem-Based Learning and incorporates important research findings from cognitive psychology. The curriculum is structured on the integration of critical concepts and each step of the curriculum is based on the growth of important concepts learned previously. The central focus of the Pre-Clerkship program is the tutorial. Tutorial problems are selected to illustrate concepts in a clinical setting and when students are exploring tutorial problems, they will be directed towards asking questions of “what”, “why” and “how”. The Pre-Clerkship curriculum is divided into five foundations: four Medical Foundations that provide an introduction to all major organ systems and an Integration Foundation that focuses on the purposeful and structurally-supported consolidation of important concepts to improve readiness for Clerkship. A novel feature of the curriculum is a horizontal Professional Competencies curriculum which runs throughout the three years of the program. There is also elective time. Learning Methods
In the Pre-Clerkship Foundations, students are presented with a series of tutorial problems, requiring the understanding of underlying biological, population and behavioural principles, the appropriate collection of data and the critical appraisal of evidence. Learning by a process of inquiry is stressed. The class is divided into small groups of 6 to 8 students, each with a tutor. In the tutorial session students develop a series of learning objectives from each tutorial case and negotiate how they will approach their learning tasks. They then acquire the knowledge and skills to meet the objectives of the Foundation in which they are working. They also learn to work as a team, helping and learning from peers. The study habits and sense of responsibility to self and others provide a basis for lifelong working and learning habits. In the Professional Competencies curriculum, students work in groups of 8 to 10, with two facilitators, one an MD, the other a clinician from an allied health care field. Learning formats include large group sessions, small group tutorials, work with standardized patients, role-plays, written projects and reflections which are collected as the student’s Reflective Physician Portfolio. To achieve the objectives of the Undergraduate Medical Program, students are introduced to patients within the first Foundation of the curriculum. In this way, students understand the relevance of what they are learning, maintain a high degree of motivation and begin to
understand the importance of responsible professional attitudes. Students admitted to the Undergraduate Medical Program have the responsibility and privilege of taking an active role in the planning and evaluation of the education program. Through representation on most policy-making and implementing committees, students can influence decisions in such areas as education, philosophy, faculty recruitment and curriculum design. It is expected that all students will participate in the continuing reappraisal and improvement of the program. Such participation is a hallmark of the Program. Student Assessment Methods
The assessment format has been designed to complement learning in the Undergraduate Medical Program. Assessment methods have been developed to measure how well the student achieves the stated educational objectives in the various components of the program. Continual assessment of students occurs within all small-group learning experiences. Students are expected to conduct self-assessment, as well as participate in the assessment of other students in their small groups. Students will also be assessed by faculty and residents, including tutors in problem-based learning tutorials, longitudinal facilitators in Professional Competencies, and preceptors in clinical skills. Several short, low-stakes assessment exercises occur during each Foundation and at regular intervals during the Professional Competencies component of the program. Tutors complete a summary of student learning progress at the completion of each Foundation reflecting student self-assessment, peer assessment, clinical skills preceptor assessment, and performance on assessment exercises, incorporating the tutor’s progress assessments throughout the Foundation.At the completion of the Foundation or the Professional Competencies assessment period, the tutor or facilitator is responsible for the final summary statement of student learning progress. Longitudinal Facilitators complete a summary of student learning progress at the completion of Medical Foundations 2, 4 and Integration Foundations based on student self-assessment, peer assessment, performance on written and skills assessments, incorporating the facilitators’ progress assessments throughout the preceding assessment period. The Professional Competencies assessment at the conclusion of the Integration Foundation serves as the final Professional Competencies assessment that will be reflected on students’ transcripts. Elective supervisors complete a summary of student performance at the completion of each elective, including as assessment of the student’s progress on achieving the proposed learning
objectives. Core clinical rotation supervisors complete a summary of student performance at the completion of each rotation. These assessment summaries reflect student clinical assessments by faculty and residents, written assessments, and assignments unique to each clinical rotation. In addition to the component-based assessment, the accumulation of medical knowledge is assessed at regular intervals by means of the Personal Progress Index. This is in a multiple-choice format. Results are available to the students for self-assessment and, in summary form, to the Student Advisor. The Personal Progress Index is in addition to, and does not replace, tutorial- and other performance-based assessment. The Program monitors student progress, and provides support for students showing persistently low progress. The acquisition of clinical and professional skills is assessed by clinical skills preceptors in each Foundation and in Clerkship. Also, students participate in an Objective Structured Clinical Examination (OSCE) on an annual basis. All student assessment data described above is available to students and their advisors via the online Medical Student Information System (MedSIS). The Program Evaluation and Student Assessment Committee (PESA) has the responsibility of working with the Medical Program to assist with the development and implementation of psychometrically sound assessment methods to provide timely and helpful information to assist students and faculty in assessing student progress. Continuation in the Program is subject to satisfactory performance. Curriculum Plan - COMPASS Curriculum
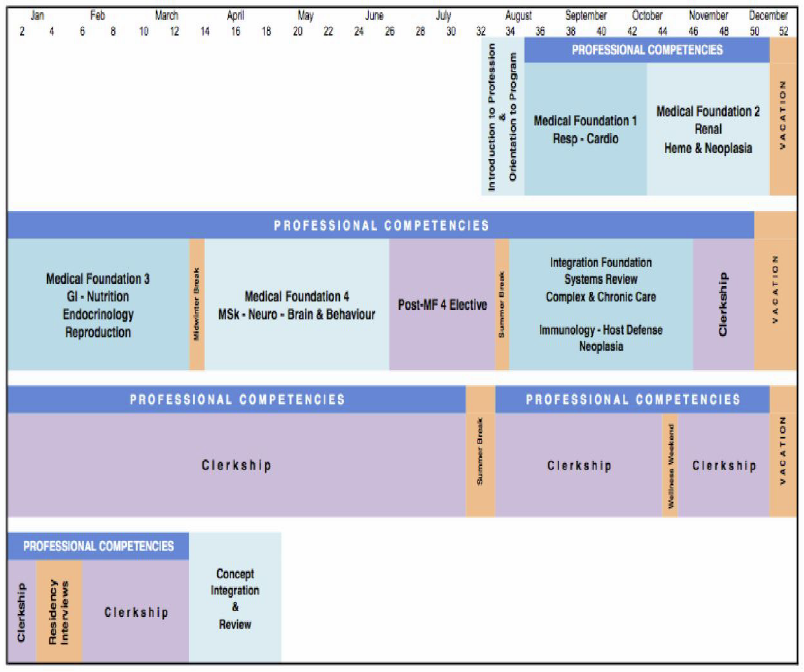 The order, timing, duration, and focus of all components of the curriculum may change in response to changing conditions with respect to the healthcare environment. Changes that occur contemporary with ongoing programming are approved by the relevant curriculum component committee, the program Curriculum Committee, and the program Executive Committee. Students will be notified of changes to the curriculum with as much notice as possible. Medical Foundation 1:
This 11-week Foundation begins with an in-depth introduction to: - areas of personal and professional development that will be required to study medicine;
- the pedagogies and assessments that are employed in the Program;
- the healthcare systems in which students will be learning and working; and
- the policies and practices of the MD Program.
Students’ knowledge- and skill-development then focuses on the respiratory and cardiovascular systems’ contributions to concepts of oxygenation and homeostasis. All students study in Hamilton for this Foundation. Medical Foundation 2:
This 8-week Foundation focuses on the renal and hematologic systems’ contribution to concepts of oxygenation and homeostasis. Students’ knowledge- and skill-development also addresses the immunologic, and neoplastic aspects of hematology. Students study in their assigned campus for this Foundation and subsequent Foundations. Following this Foundation, students have a two week break from study. Medical Foundation 3:
This 12-week Foundation focuses on concepts of energy, homeostasis, and reproduction through knowledge- and skill-development that centers on the digestive, endocrine, and reproductive systems. Following this Foundation, students have a one-week break from study. Medical Foundation 4:
This 12-week Foundation focuses on concepts of locomotion and of neurosensory and behavioural responses to the environment through knowledge- and skill-development that centers on the musculoskeletal system, the neurological system, and psychiatric (brain & behaviour) medicine. Following this Foundation, students will take 7 weeks of clinical electives and two weeks of holidays throughout the first summer of the program before beginning the Integration Foundation in late August of second year. Integration Foundation:
This 12-week Foundation focuses on review of key concepts from the four Medical Foundations in the context of - complex, multi-system diseases;
- chronic illness; and,
- concepts centering on immunology, host defense, and neoplasia.
The Integration Foundation allows students to consolidate medical concepts and skills, clinical skills, and professional competencies, offering an opportunity to enhance clinical transfer and support students’ transition to and readiness for Clerkship. Professional Competencies
The Professional Competencies curriculum is longitudinal. There are seven learning domains of this component of the curriculum: effective communication; population health and its determinants; interprofessional education; medical decision-making; moral reasoning and ethical judgment; professionalism and self-awareness; and social, cultural, and humanistic dimensions of health. The Professional Competencies curriculum is a safe learning lab for the acquisition of the dynamic and fluid reasoning and interpersonal skills required to be a physician. In their groups, students have the chance to practice many skills. During the Clerkship, the curricular content relating to the Professional Competencies domains becomes integrated into the core teaching in each clerkship rotation and is developed by the clerkships in their own formats. Clerkship
Clerkship is the prime opportunity for students to participate in the direct care of patients while continuing to learn the knowledge, skills and attitudes required to become a physician. The Clerkship curriculum is firmly linked to the Pre-clerkship concept-based curriculum and includes continuation of the Professional Competencies curriculum. The student moves from tutorial cases developed around simulated patient scenarios to experiencing the care of real patients and populations. Students integrate their skills of learning and assessment into the hospital and clinic environments. Students experience three phases of Clerkship: Transition to Clerkship, Clerkship Foundations, and Transition to Residency. The core and electives rotations occur in the last two phases. Students continue to have periods of dedicated teaching time throughout the core clerkship program in all three phases. This clerkship-specific curriculum delivery includes: large group sessions, small group tutorials, in-person and virtually-delivered sessions, on-line modules, and guided self-study. Students begin with Transition to Clerkship in Fall. Students move into Clerkship Foundations, which consists of 42 clinical weeks: seven 4-week core rotations (Internal Medicine, Surgery,
Family Medicine, Psychiatry, Pediatrics, Obstetrics and Gynecology, and Emergency Medicine), two 2-week cores (Anesthesia and Orthopedic Surgery) and six 2-week electives.
The Clerkship Foundations program has six 2-week Clerkship Electives to allow students to hone their skills an explore a variety of clinical areas as well as have the opportunity for dedicated research time. Transition to Residency (TtR) consists of 16 weeks of rotations and will begin after the Clerkship Foundations ends. Students in TtR will have an opportunity to function as “senior” clinical clerks. These two-week rotations will focus on ensuring students have generalist “residency-ready” clinical skills, knowledge, and attitudes within each of the TtR rotation areas (Specialty Selectives, Internal Medicine, Surgery, Pediatrics, Family Medicine, Psychiatry and two 2-week Electives). The Clerkship rotations take place in hospitals and clinics in the Hamilton, Niagara, Waterloo Regional Campuses as well as the MacCARE Clinical Education Campuses: Grand Erie Six Nations, Burlington, Halton and Osler. In the winter of their third year of medical school, students have a three-week break aligning with the national residency interview period. Electives
Elective studies form an integral part of the Curriculum Plan. They may be considered the epitome of self-directed learning, since students must define goals for electives which are appropriate for their own learning objectives. These objectives represent specific areas of educational need or interest. The responsibility for planning electives rests with each student in collaboration with the student advisor. The two types of electives in the Undergraduate Medical Program are: - Block Electives: These are blocks of curriculum time dedicated to full-time elective activities. Their satisfactory completion is a mandatory component of the Undergraduate Medical Program. Block Electives occur after Medical Foundation 4 and during the Clerkship, for a total of 23 weeks. To achieve disciplinary diversification, students must adhere to the National Diversification Policy.
https://www.medportal.ca/sf-docs/default-source/electives/ug-national-electives-diversificationpolicy.pdf?sfvrsn=fe381b4f_6electives/electives_diversification_policy.pdf?sfvrsn=4 - Horizontal Electives: These observership/shadowing experiences are undertaken concurrently with other parts of the curriculum during pre-clerkship after students have completed a mandatory Longitudinal Family Medicine Experience which occurs within the first half of the first year. Horizontal electives are entirely optional, not being required for completion of the program, but are used to explore or review a specific area of knowledge or practice in more detail.
It is particularly important that the student’s advisor be involved in all decisions concerning the selection and carrying out of horizontal electives. Concept Integration and Review (CIR)
Concept Integration and Review (CIR) is the final course of the Program spanning 5 weeks. It begins with one week after the residency interview break and continues for 4 weeks after the last Transition to Residency Clerkship blocks. The goals of the block are to help students review and synthesize important concepts that are essential for transitioning to postgraduate medicine programs and to help prepare students for the MCCQE Part 1 Licensing Exam through concept review and exposure to test-taking strategies. Dedicated self-study time throughout the block is provided and students are expected to review content prior to attending scheduled sessions. Large group sessions focus on highlighting key concepts and test-taking skills are provided by content experts. Enrichment Program
The purpose of the Enrichment Program is to stimulate an interest in research and scholarly activity among medical students and to attract some to careers in academic medicine and medical research. These experiences will not normally begin until the Pre-Clerkship is completed. Applications will not be considered for the Post-Clerkship period. MD/Ph.D. Program
The McMaster MD/PhD Program has been training future clinician-scientists since 2007. The rapid pace of healthcare-related research and discovery requires exceptional people who are trained to bridge the gap between basic sciences and clinical application. The McMaster MD/PhD program combines the strength of a unique, patient-oriented medical education with a strong, internationally renowned healthcare research environment. At present time, students enrolled in the MD/PhD program may carry out the PhD component of their studies in one of the following graduate programs affiliated with the Faculty of Health Sciences at McMaster University: Medical Sciences, Biochemistry, Health Research Methodology, Neurosciences, Biomedical Engineering, Chemical Biology and Health Policy. Minimum criteria for admission is a 4-year Honours BSc or BHSc with a Grade Point Average (GPA) of 3.8 or greater on a 4 point scale in the final two years of Bachelor’s degree study (with an overall 4-year GPA of at least 3.00/4.00), and a score of 127 or higher on the Critical Analysis and Reasoning (CARS) section of the MCAT. The MCAT must be written within five years of the application year. Please note that McMaster will use the most recent MCAT score for those who write the MCAT more than once. As some PhD programs may have additional requirements specific to their program, applicants should review the relevant sections of the McMaster School of Graduate Studies Calendar. Eligible students will have a proven record of research involvement at the undergraduate or graduate level. Existing in-program Master’s students or students in their first year of PhD training in an eligible Health Sciences Affiliated Graduate program at McMaster University are also welcome to apply to the MD/PhD Program with the written consent of his or her research supervisor. Students from other Universities may apply if they will finish their graduate degree requirement before enrolling in the McMaster MD/PhD program. Existing McMaster MD students with a strong research background are also welcome to apply in their first year of medical school.
To apply to the MD/PhD Program, applicants must submit a separate application in the McMaster Graduate Studies Application Portal (Slate), in addition to the OMSAS application. To gain admission, applicants must be accepted to both the MD Program at the Michael G. DeGroote School of Medicine and one of the PhD programs listed above. Application to the MD component is through OMSAS and must be submitted by the deadline they set. The PhD component of the application is due on November 1st of the application year. Further information and the PhD application can be found at: http://fhs.mcmaster.ca/mdphd/ Regulations for Licence to Practise
A degree in medicine does not in itself confer the right to practise medicine in any part of Canada. To acquire this right, university graduates in medicine must hold a certificate of the College of Physicians and Surgeons of the province in which they elect to engage in practice. Post-graduate learners (residents) in Ontario will be required to register with the College of Physicians and Surgeons of Ontario (CPSO). Students intending to practise outside Ontario are urged to consult the licensing body of that province regarding registration as residents. Licensing requirements vary somewhat among the provinces. The current Ontario requirements for issuance of a Certificate of Registration Authorizing Independent Practice are: - Certification by the Royal College of Physicians and Surgeons of Canada or the College of Family Physicians of Canada;
- Parts I and II of the Medical Council of Canada Qualifying Examination;
- Canadian Citizenship or Landed Immigrant Status.
Canadian Resident Matching Service (CaRMS)
The Matching Service is a clearing-house designed to help final year medical students obtain the post-MD program of their choice, and to help program directors obtain the students of their choice. It provides an orderly method for students to decide where to train and for program directors to decide which applicants they wish to enroll. For both students and directors, it removes the factors that generate unfair pressures and premature decisions. In the winter of their third year of medical school, students have a three-week break aligning with the national residency interview period. Basic Life Support Training
All students are required to provide evidence of a current Basic Life Support (BLS) for Health Care Providers (C) certificate (i.e. Red Cross CPR/AED Level HCP; St. John Ambulance Level C HCP; Heart and Stroke BLS for Healthcare Provider C) by July 31st of the year of entry. Information is sent to successful applicants prior to registration. The cost of this course is the responsibility of the student. Courses are readily available in most communities. Health Screening
Learners in the Undergraduate Medical Education Program will participate in courses which include clinical activities with direct patient contact and standardized patients and are therefore required to complete the Faculty of Health Sciences health screening requirements prior to program start as well as annual updates during the program. Failure to do so will result in suspension of clinical activities. Information will be sent to successful applicants prior to registration. For more information, see: https://fhs.mcmaster.ca/healthscreening/ Police Records Check
Through the course of their medical school program, all medical students will serve vulnerable populations. In an effort to protect these vulnerable people against potential risk of harm, the Ontario Faculties of Medicine and many clinical agencies require that all medical students provide an annual Vulnerable Sector Check (VSC). As a condition of continued registration, students must submit an original VSC by July 31st of their incoming year and in each academic year for which they are registered. VSCs are site specific therefore McMaster University must be listed as the requesting institution. A Vulnerable Sector Check will include the following information: - Criminal convictions from the National Canadian Police Information Centre (CPIC) database and/or local databases
- Summary convictions, for five years, when identified
- Findings of Guilt under the Youth Criminal Justice Act within the applicable disclosure period and only for persons applying for a position with a government agency (federal, provincial, municipal)
- Outstanding entries, such as charges and warrants, judicial orders, Peace Bonds, Probation and Prohibition Orders
- Absolute and conditional discharges for 1 or 3 years respectively
- Non-conviction dispositions including, but not limited to, Withdrawn and Dismissed and where it meets the Exceptional Disclosure Assessment
- Not Criminally Responsible by Reason of Mental Disorder
- All record suspensions as authorized for release by the Minister of Public Safety
Files of applicants who have presented a Not Clear Vulnerable Sector Check will result in consideration by the Police Records Check Advisory Panel as outlined in the FHS Police Record Check Policy
(https://fhs.mcmaster.ca/pcbe/documents/FHSPoliceRecordCheckPolicyJune262019.pdf). Laptop Requirement
The MD Program delivers lectures, course materials, and assessments online and communicates with students and faculty between the three campuses through the use of email as well as various software programs, including web conferencing and exam applications. Thus, the MD Program requires that each student own a PC or Apple laptop running an up-to-date Windows or Apple operating system with webcam capabilities while attending the program. Transportation Costs
Students are expected to travel outside their home campus area for mandatory teaching sessions, clinical placements and clerkship rotations. Students are responsible for their own transportation and associated costs in order to complete program requirements. It is anticipated that further rotations will be developed in rural, under-serviced and remote areas. In certain cases, there will be some external funding available. For students who are accepted into the Waterloo Regional Campus and the Niagara Regional Campus, curriculum will begin within the regional campuses with some common educational experiences in Hamilton. Students will be expected to cover the cost of commuting and/or accommodations. Program changes in response to changing healthcare environment may alter these arrangements. Students will be notified of such changes with as much notice as possible. Each Regional Campus is approximately a one-hour drive from Hamilton. The elective experience can be spent in various activities utilizing local, regional or distant resources. Students are expected to cover all transportation and associated costs for electives. Funding may be available for elective travel expenses through a number of funding programs. Admission Policy for the Undergraduate Medical Program
The official admission policy and deadlines for the Undergraduate Medical Program shall be as published in the Ontario Medical School Information Booklet. This booklet is available through: Ontario Medical School Application Service (OMSAS)
170 Research Lane
Guelph, Ontario, N1G 5E2
(519) 823-1063
http://www.ouac.on.ca/omsas
omsas@ouac.on.ca Please note that the admission policy is reviewed annually, and the admission requirements from the previous year may not apply. Because of the nature of the selection procedures, deadlines are strictly enforced. All relevant documentation must be provided by the specified deadlines. Applicants must follow the instructions precisely. All applicants should be aware that the Admissions Office is committed to the protection of personal information. Use of personal information is strictly limited to the appropriate handling of applications, record-keeping for those admitted to the program, and research intended to further the efficacy of Medical Education Program procedures. The University reserves the right to change the admission requirements at any time without notice. Admission and Registration Registration in the Undergraduate Medical Program implies acceptance by the student of the objectives of the program, and the methods which evaluate progress toward the achievement of those objectives. The following describes the regulations governing admission and registration in the Undergraduate Medical Program. The final application deadline is October 1st. The deadline is strictly enforced. Admission Policy and Procedure The intention of the McMaster Undergraduate Medical Program is to prepare students to become physicians who have the capacity and flexibility to select any area in the broad field of medicine. The applicant is selected with this goal in mind. Faculty, medical students and members of the community are involved in the admissions process. Application to the medical program implies acceptance by the applicant of the admission policies and procedures, and the methods by which candidates are chosen for the program. Applicants who will not be ready or able to begin studies as expected may withdraw their applications without prejudice. Application fees cannot be refunded. Several hundred applicants will be invited for an interview in March or April. From this group a class of 203 is selected. All applicants are notified in writing, by McMaster University, of the results of their application. These letters will be sent electronically to applicants on the second Tuesday in May. Falsification of Admission Information Applicants should understand that where it is discovered that any application information is false or misleading, or has been concealed or withheld, the application will be deemed to be invalid. This will result in its immediate rejection. If the applicant has already been admitted and registered as a student, withdrawal from the University may be required. The MD Admissions Committee will normally not allow the applicant to reapply to the Medical Program for seven (7) years. Essential Skills and Abilities Required for Entry to a Medical Degree Program The Ontario Faculties of Medicine are responsible to society to provide a program of study that graduates Doctors of Medicine with the knowledge, skills, professional behaviours and attitudes necessary for postgraduate medical training and independent medical practice in Canada. Graduates must be able to diagnose and manage health problems and provide comprehensive, compassionate care to their patients. For this reason, students in the MD program must possess the cognitive, communication, sensory, motor, and social skills necessary to interview, examine, and counsel patients, and competently complete certain technical procedures in a reasonable time while ensuring patient safety. In addition to obtaining an MD degree, and completing an accredited residency training program, an individual must pass the licensure examinations of the Medical Council of Canada (MCC) in order to practice medicine in Canada. Therefore, MD programs have embedded expectations of both knowledge- and skills-based competencies. Prospective candidates should be aware that cognitive abilities, physical examination proficiencies, management skills, communication ability, and professional behaviours are all evaluated in timed simulations of patient encounters. All students must therefore have the required skills and abilities described in the Section on Technical Standards. These are standards that are necessary for success in the MD Program, and to be sufficiently competent to participate in supervised residency training. All individuals are expected to review this document to assess their ability to meet these standards. The document can be found at https://mdprogram.mcmaster.ca/md-program-admissions/who-should-apply. Academic Eligibility Requirements All applicants must fulfill the requirements described below: - By May of the year of entry, applicants must have completed a minimum of three years of undergraduate work. To satisfy the minimum requirements, academic credentials obtained from a Canadian University must be from an institution with academic standards and performance consistent with those of member institutions of the Council of Ontario Universities (COU). The applicant must be able to demonstrate a high level of academic achievement consistently throughout their undergraduate career.
- A minimum of 15 full-courses, or 30 half-courses (three years) of Undergraduate university work from a recognized university is required. There is no requirement that applicants carry a full course load. Marks from supplementary and summer courses will be included in the grade point average calculation. If requested, applicants must provide evidence that this requirement has been met by May 30th of the year of entry. Courses graded only by the assignment of Pass or Credit are counted for credit, but will not be included in the GPA calculation. In this case, a minimum of five half-year or five full year courses with letter or numerical grades is required.
- An applicant who has completed a diploma at a CEGEP must have completed by May of the year of entry, at least two additional full academic years of degree credit work at an accredited university.
- Applicants who have completed the requirements for a baccalaureate degree in less than three years by the October 1st deadline, are also eligible.
- By October 1st, applicants must have achieved an overall simple average of at least a 3.0 on the OMSAS 4.0 scale. While an overall simple average of at least 3.0 on the OMSAS 4.0 scale meets the minimal criterion for consideration for admission, prospective applicants should be aware that given the rapidly rising level of competition for a limited number of positions, a significantly higher GPA would provide them with a more reasonable chance of admission. Due to changes from year to year in the level of competitiveness, an exact figure in this regard cannot be provided.
- Medical College Admissions Test (MCAT) - The MCAT is required for application and must be written within five years of the application year. The score from the Critical Analysis and Reasoning section will be used in both formulae (offer of interview and offer of admission). A minimum score of 123 on the Critical Analysis and Reasoning component is required. All other MCAT component scores will not be considered in the selection process. For those applicants who write the MCAT more than once, the score from the most recent MCAT will be used.
- Computer-based Assessment for Sampling Personal characteristics (CASPer): All applicants to the Michael G. DeGroote School of Medicine, McMaster University will be required to complete a 90 minute computer-based test, called CASPer, as part of the selection process. CASPer is a web-based assessment of interpersonal skills and decision-making, to be completed at a computer. Applicants must register for CASPer, which is offered in the Fall of each application year, at https://acuityinsights.app/.
No other aspects of the application will be considered if these requirements are not met. Indigenous Applicants With an understanding that Indigenous learners can face specific barriers or challenges when pursuing higher education, schools and programs within McMaster’s Faculty of Health Sciences have facilitated admissions streams for applicants with Indigenous North American (First Nations, Inuit or Métis) ancestry. This process is intended to provide equitable access to Indigenous applicants and aligns with the intent of the Truth and Reconciliation Commission of Canada Calls to Action. Applicants wishing to apply through McMaster’s FIAP need to complete the self-identification application in addition to the McMaster University and program specific application processes. The FIAP application is submitted to McMaster’s Indigenous Health Task Force (IHTF) through the ISHS office website. Information on the policy, application requirements and the online application can be found at: https://ishs.mcmaster.ca/admissions/self-identification. One self-identification application is used for all Faculty of Health Sciences programs that have a facilitated Indigenous admissions stream, and should only be completed once even if an applicant is applying to multiple programs. Applicants identify the program(s) they are applying to on the Self-identification Application. The applicant is responsible for ensuring the Self-identification Application is submitted by the application deadline(s) for the program(s) they are applying to in addition to completing any other application required for that program(s). If applicants are applying to multiple Faculty of Health Sciences programs, the Self-identification Application must be completed by the earliest deadline date. Indigenous applicants are also required to complete the Undergraduate MD Program application package as provided by the Ontario Medical School Application Service (OMSAS). Applicants must meet the same minimum academic criteria for admission as described in the “Academic Eligibility Requirements” section. * In order to reduce barriers for Indigenous applicants, provision of MCAT critical analysis and reasoning score may be deferred beyond October 1st. Those Indigenous applicants wishing to delay taking the MCAT until after invitations to interview are sent out are free to do so, but should be aware that they MUST forward a minimum MCAT critical analysis and reasoning score of 123 or higher to the Admissions Office by the offer date (the second Tuesday in May), in order to maintain eligibility. Indigenous applicants wishing to explore this option should book their MCAT in the Fall to be certain of a spot. A cancellation fee would be applied by MCAT if the applicant is not successful in obtaining an interview and subsequently cancels their MCAT test. Black-Equity Stream (BESt) As a part of McMaster’s Michael G. DeGroote School of Medicine’s commitment to equity in medical school admissions, a Black-Equity Stream was introduced for the 2022/23 application cycle. This process is intended to provide equitable access to Black applicants and aligns with the McMaster MD Program’s commitment to the principles of equity, diversity, inclusion and social justice in all that we do, and McMaster University’s statement on Building an Inclusive Community with a Shared Purpose https://secretariat.mcmaster.ca/university-policies-procedures-guidelines/. All the applicants applying through BESt are required to complete the Undergraduate MD Program application package as provided by the Ontario Medical School Application Service (OMSAS) by the specified deadline, where they will self-identify to indicate their interest. A supplementary application which will accompany their application, consisting of a personal essay from the applicant to describe their interest in applying through the BESt, is also required. Applicants must meet the same minimum academic criteria for admission as set out for the general pool of candidates. Geographical Consideration The geographical status of the applicant is determined from the Autobiographic Sketch. Applicants may be asked to provide evidence of geographical status. In selecting applicants for interview, the bona fide place of residence will be based upon: 1) the province of Ontario; or 2) the rest of Canada and other countries. To qualify for Ontario status, an applicant must be a Canadian citizen or permanent resident of Canada by October 1st, and have resided for at least three years in the province of Ontario since the age of 14 by the date of possible entry into the program. Transcript Requirements and Transcript Request Forms (TRF) All transcripts must be ordered by OMSAS via the Transcript Request Form (TRF) where that procedure has been established. Applicants must request all other transcript materials prior to September 15th, to allow adequate time for processing requests and for receipt at OMSAS by the prescribed deadline. If an applicant is registered at a post-secondary institution at the time of the application deadline and that registration is not reported on the transcript, the applicant must arrange to have the Registrar of the institution send a Statement of Registration to OMSAS by October 1st. This statement must indicate the in-progress course name(s) and number(s). Evidence to show that applicants requested transcripts and Registrar statements in a timely fashion may be requested by McMaster University. Applicants should retain all receipts and correspondence related to their transcript request. It is entirely the applicant’s responsibility to ensure that all of the above are received at OMSAS by October 1st. Failure by the applicant to meet these requirements will result in the disqualification of the application. All transcripts must be submitted directly to OMSAS by the post-secondary institutions attended. McMaster requires that applicants provide transcripts of all courses/programs attended at any post-secondary institution. This includes community colleges, CEGEPs, junior colleges, pre-university programs, etc. Failure by the applicant to comply with the instructions or to meet the deadlines will result in disqualification of the application. Graduate Students Those applicants with a completed and conferred Master’s or Ph.D. at the time of application will receive a small amount of extra weighting in the formula used to determine the likelihood of invitation to an interview. Individual grades for course work taken as part of a graduate degree will not be included in the calculation of the grade point average. Graduate students enrolled in a graduate program at the time of application must arrange for their Supervisor, a member of their Supervisory Committee, or the Chair of the Department to provide a letter indicating they are aware the applicant is intending to apply to medical school. Applicants should arrange for this letter to be received at OMSAS by October 1st. If the applicant’s graduate degree supervisor is acting as one of their references, a second letter is not required. Credentialing of Non-Canadian Grades Applicants, Canadian or non-Canadian, who have not met the minimum course number criterion utilizing their Canadian data and require inclusion of their international education data to meet the minimum course number criterion are required to have their foreign transcript assessed by World Education Services (WES). Credentialing assessment means converting foreign academic credentials into their Ontario educational equivalents. A course-by-course evaluation along with the calculation of an overall GPA is required. Applicants must have their transcripts sent directly from their university to WES and OMSAS and be able to prove (with dated letter and dated post office receipt) that an attempt was made to have the transcript issued by their university and sent to OMSAS by October 1st. Those requiring WES assessment must also ensure that transcripts are received by WES in time for their assessment to reach OMSAS by October 1st. A WES Assessment is not required for courses or programs completed on foreign exchanges. English Language Proficiency Applicants whose first language is not English must satisfy by October 1st, at least one of the following conditions: - Provide evidence of a combined score on the TOEFL iBT test with an overall score of at least 86 with minimum scores of 20 in each of the four components, or the equivalent on other recognized tests has been achieved (McMaster University code for TOEFL test score submissions is #0936); or
- Have attended an educational institution, where instruction was in English, for at least three years; or
- Have resided for at least four years in an English-speaking country.
Interviews Several hundred applicants will be invited to interview. The interview process entitled the Multiple Mini Interview (MMI), is primarily composed of a series of 8-10 ten-minute encounters over a two-hour period. For the 2022-2023 application cycle, the MMI will be held virtually. Selection All the information resulting from the process described above, as well as the Confidential Assessments from referees, may be reviewed and used in the final selection. Applicants will be notified in writing, by McMaster University, of the results of their application. These letters are sent electronically to applicants on the second Tuesday in May. Anyone accepting an offer of admission must provide, within two weeks of acceptance, a deposit in the amount of $1,000 (Canadian), non-refundable, which will subsequently be applied towards tuition. The MD Program begins in early-August. Students accepting their offer of admission must be available to begin the program on the schedule start date and must attend all day-time program-related sessions. Application for Deferred Registration Deferred registration may be granted only under exceptional circumstances. The request for deferral must normally be submitted within two weeks of the offer of admission and will be considered by the UGME Deferral Board. Deferral for parental/family, illness or other personal/compassionate reasons may be considered if received after this deadline where circumstances did not allow the applicant to meet the deadline. International Applicants Interested International applicants may apply through the regular process. International (Visa) students should be aware that admission to the Undergraduate MD Program does not confer eligibility to apply subsequently through the Canadian Residency Matching Service (CaRMS) for a residency training position in Canada. Applicants should check the CaRMS web site (http://www.carms.ca/) for further information. Applicants Currently or Previously Registered in a Canadian or US Medical School Typically, the Michael G. DeGroote School of Medicine, McMaster University, does not admit students registered (currently or previously) in medical school in Canada or the United States. Should an applicant wish to pursue admission in this case, the Admissions Committee will require a letter outlining the extenuating circumstances guiding the application to McMaster. The letter should clearly address why the move to a new and different medical school is necessary, compelling, and unable to be addressed at the current/previous medical school. The Admissions Committee reserves the right to investigate and confirm the claims made in the letter. This may include contacting the current or previously attended medical school. Advanced Standing/Transfer The structure of the McMaster Program requires that all students begin in Medical Foundation 1. There is no provision for advanced standing or transfer into the program. Unsuccessful Applicants Application files, including transcripts, from one year are not held over to another year. If an unsuccessful applicant wishes to reapply, a new application package, including supporting documentation must be submitted, using the OMSAS Application and the OMSAS Information Booklet, for the new admission selection cycle. Retention of Documents All documentation submitted in support of an application for admission becomes the property of the University and is not returnable. If an applicant is not accepted, or fails to enroll following acceptance, the identifiable documentation will be destroyed at the end of the admissions cycle in keeping with university policy. Financial Information
Financial difficulties are among the most frequent problems experienced by students in undergraduate medical schools. At McMaster, these are intensified by the lack of opportunity for summer employment. In this situation, it is incumbent on students admitted to the MD Program to clarify immediately their personal financial situation and to secure or identify sufficient support to meet their financial obligations over the subsequent three years. The Undergraduate MD Program cannot assume this responsibility. In 2022-2023, the academic fees (tuition and student supplementary fees) for a student in the McMaster Undergraduate Medical Program were: Canadian Citizens and Landed Immigrants | Year I | $26,155.32 (OOP $28,203.40) | | Year II | $26,155.32 (OOP $27,411.81) | | Year III | $26,155.32 (OOP $26,155.32) | International (Visa) Students In addition, the cost of books and diagnostic equipment for a Year I student was approximately $3,000. It is strongly recommended that students purchase the full complement of medical equipment necessary for clinical skills. Equipment lists and special prices will be offered to medical students within the first few months of medical school. Students are also responsible for their transportation costs related to their training. Financial assistance is available to Ontario residents from the federal and provincial governments through the Ontario Student Assistance Program (OSAP). To be eligible a student must be a Canadian Citizen or permanent resident of Canada and fulfill certain requirements for residency in Ontario. Students who are legal residents of other provinces need to check with their respective provincial financial aid programs about eligibility for support prior to acceptance. In addition, the following sources of funding are available to undergraduate medical students: Bursaries There is a bursary program which has been developed by the Faculty of Health Sciences and the central University campus. Bursaries are awarded to students who are Canadian citizens and demonstrate financial need. All bursaries are distributed during the late fall of each year. Bursaries are intended to offset provincial financial assistance and cannot supplement the full cost of medical education. The Undergraduate Medical Program has in the past indicated its preparedness to recognize students who distinguish themselves and the University by virtue of their scholarship and their contribution to the university community. At the same time, the School has indicated that the terms of reference for such awards should neither compromise the spirit of cooperative scholarship which characterizes its MD Program nor replace its priority of concern for assisting those students with the greatest financial need.. A growing number of estates and agencies have donated funds to the University and the Undergraduate Medical Program for purposes of recognizing scholastic merit among medical students. In order to meet the requirements of these awards within the spirit of cooperative scholarship, these funds are available to support individual students in their pursuit of specific elective projects or activities. MD Program Donor Bursary applications can be accessed through AwardSpring during the annual UGME Bursary Program in September/October. |
 Return to: Programs (by Degree) and Minors Return to: Programs (by Degree) and Minors
|
|
| |